A Q&A session with Maryline Mulemba, MSF Head of Mission in Malawi and Testimonies from Antiretrovial Program Patients
MSF's Triple Therapy Program Patient inclusion criteria:
Treatment process:
Intake per month: 20 people, or five patients a week. At the end of September, 27 patients had benefited from triple therapy. |
In Malawi, 800,000 people are thought to have HIV/AIDS, of which 40,000 are children and 420,000 are women, many of whom are of childbearing age. About 10% of the population (16% of the adult population) is HIV-positive.1
MSF's triple therapy treatment program for AIDS patients began in August 2001, and was developed as part of the larger MSF AIDS project in Chiradzulu hospital. The program is run by a medical and paramedical team and provides medication support, materials, financing and reestablishment of a nutritional center, and an anonymous, free testing center.
After several months of preparation, MSF's HIV/AIDS triple therapy treatment program in Malawi started in August 2001, at the same time that the Malawi government registered several antiretroviral drugs. Setting up the program was not a problem-free process. We found out what is happening today in an interview with Maryline Mulemba, head of mission in Malawi.
What, to you, is the single most important message to send about ARV treatment and AIDS in Africa?

We need to send a more hopeful picture. Let's talk about the ones who live with AIDS instead of the ones who died of AIDS.
Do you think that by portraying images of Africans taking the ARV treatment and feeling better we can motivate people to be more proactive about funding treatment?
Yes, because if you can show people taking the drugs and who are ok, then what would stop governments from giving them the drugs? Now, when you think about drugs, there are still a lot of people who say, "They are not going to take it, they are not going to be compliant." Even among the community, it's hard to see everyone dying of AIDS. But if they see people with AIDS healthy and living with the disease, then it changes the way they think of AIDS.
Before the start of the program, people expressed many concerns and worries. What is the situation today?
We are the only district where something is happening for HIV on the ground, where everybody can have counseling and testing if they want, the blood is clean, there is IV in the hospital that there is good quality of care in the hospitals. And that is good for the population. It's not like that in the rest of the country.
Their concerns were mostly about our patient admission criteria. For instance it was suggested we should choose only women, because they are the ones who bring up the children. This would enable us to reduce the risk of transmission. But what if a woman loses her husband? How will she survive alone with her children, without any money? That's why we decided to set up a "selection committee", which decides on admissions in partnership with the ministry and local staff. Because people wondered for example how we would manage to resist political pressure—how do you say no to an express request from a minister?
There are two types of criteria for patient inclusion in the program. The first are medical criteria: patients must have a CD4 count below 200. Then there are non-medical criteria. For the moment, we are only working in Chiradzulu hospital. Patients must be able to walk to the hospital. Each patient must also be assisted by a "guardian" who accompanies him or her to the daily visits and follows the medication. The presence of this guardian implies that the patient has made the active step of telling someone (s)he has AIDS. We realize this may pose ethical questions. But it is hard for a person to take medication twice a day without anyone knowing. Also, in the case of a couple where one is receiving ARV treatment and the other hasn't been tested, it can encourage the patient to talk to his or her partner and give him or her what may be vital information. And some patients may have side effects—it's useful for them to have someone nearby who knows about their treatment.
A few weeks into the ARV treatment program, what are your first impressions?
Before we started ARVS, the group of people with AIDS had a lot of difficulty speaking about their status. Now they are feeling good, they have changed their image, looking healthy, working and contributing to their community. Now it's very easy to say, "I've got AIDS, but I'm fine." This would have never happened before the drugs, because they would have died of it.
We haven't been confronted with the difficult choice of which patients to include in the program, because we've been able to give treatment to all those who needed it. We haven't yet noticed any problems with compliance—patients seem to be taking their treatment well. Out of all the patients on triple therapy, only a few had minor side effects, such as nausea. None have had to stop treatment so far. We now have thirty or so patients on ARV, all adults. We take on five more patients every week. Our final goal is to have 500 patients admitted to the program.
How are the patients?
Most of them have already started to put on weight again! Some look really well, even though their CD4 level is at 1! But their physical state is not a real reflection of their illness. They don't actually have a choice. It's even a question of survival: most of them can't possibly stay in bed, they absolutely have to work. In any case it's still too early to talk about "spectacular" results. Let's just say it's encouraging. Psychologically though, it's very important for the teams to start seeing the effect of the treatment. But in a few months, some patients who are better may ask themselves "why do I need to keep taking these medicines?" Compliance is difficult at the start, but it's even harder after six months. We'll keep on seeing them once a month or once every three months if they're very compliant, just like it's done in Europe.
Will the treatment and follow-up plan evolve?
At the moment, the treatment procedure is very complicated for the patient; in fact it's a real battle. But when the program was first set up, no one knew exactly how things were going to work, so our organization was rather complex. For instance we decided to have five or six meetings with the team before the start of each treatment, followed by one compulsory visit every week for eight weeks. We're going to change that to two first visits, one two weeks later, followed by a monthly visit from then on. We'll still promote the guardians, but it won't be compulsory anymore, especially for those who visit the HIV/AIDS clinic regularly. In 2002, we plan to start admitting patients for triple therapy in other health centers in the district. After that, we'll start including patients who are already hospitalized and can be followed within the health centers. Simplifying our organization will enable us to admit many more patients. Once we've reached 500, we'll reassess.
You also offer treatment for local staff working with MSF?
It's different for them. They're covered for ARV treatment by their staff insurance. They go to the reference hospital, where they're followed by a doctor. They have to have a CD4 count lower than 200, but all our staff and their families have a right to treatment. In January, we had a meeting to remind them that treatment was being offered to them, but only ten people out of fifty or so actually got tested. I had fought to obtain ARVs for them, and I was convinced I would never again have to bury a member of my staff—how naïve of me!
Are patients receiving ARV treatment stigmatized?
Malawi is a society of taboos. The country claims it is "God-fearing", that its society is based on firm morals and family values, sexuality within the marriage… all these Christian notions which everyone seems to adhere to, but which in fact no one respects. For instance extramarital relationships are common. AIDS patients do stay within their family, there's no real exclusion as such. And in hospitals, AIDS patients are treated just like everyone else. But no one talks about it, so it's very difficult for people to say they are HIV-positive, even if everyone knows it. Officially, no one here dies of AIDS. ARVs may help patients who are well to assert themselves as persons living with AIDS. That will be a victory.
The collective denial of the illness is one of the main reasons for the explosive AIDS epidemic in Malawi. Malawi doctors don't tell patients they have AIDS because they don't have treatment to offer them. This has to change. If you don't say you have AIDS, you're in denial—so you don't protect yourself. In this health system, people are sent home and continue to have unprotected sex. They go on putting their wives and possible others at risk, and they have children without realising the consequences. These people are real "time bombs".
Are you thinking about including children in the ARV program?
At the start, we chose to only treat adults—at least until we gained sufficient organizational experience. Now we can start including children. If some of our patients have children who are sick, they will be priority. We'll also include children admitted to the nutritional center who don't improve after three weeks. Then we'll pick up our testing of 18-month-old children of HIV-positive mothers. Or one-year-olds if they're sick—we'll check their CD4 levels. We just need to order pediatric treatment formulations, especially syrups.
What are the first reactions to the program?
The Malawi authorities have been very involved. The health ministry's number two and three came to visit the program and they had a very constructive approach. In fact they're now negotiating with Cipla to get drugs. The aim of our program is to treat 500 people with ARVs, but also to encourage other partners and the government to expand the project. With Cipla's offer, we'll be able to increase access. Treatment now costs $600 for a year (or 3,000 kwatchas per month) whereas it used to cost 10,000 kwatchas per month for combination therapy in Malawi. Large private companies may already be interested; they could include ARVs in their medical coverage, because many of their staff are affected by AIDS—and die because they don't get treated, because they can't afford it. That's our program's "snowball" effect. We treat patients and show that it's possible. That's all you need to do.
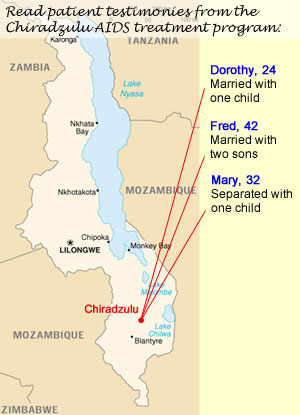
Testimonies from Patients in the Chiradzulu Triple Therapy Program

An MSF staff member cares for a patient at Chiradzulu. |
Dorothy2
Dorothy is 24 years old, although she looks 16. This thin and pretty woman is married and has an 18-month child. She lives in Massanjala, a village in the Chiradzulu district. It was tuberculosis that first took her to Chiradzulu hospital, where she was tested for HIV. It's been 8 weeks since Dorothy first started her ARV treatment, but she is still coughing a lot.
"I was coughing a lot, so in May 1999 I went to the hospital to get treatment. It was then I was advised to do an HIV test. I stayed in hospital for two months to be treated for tuberculosis and I got the results of my test one week after my arrival. When I found out that I had AIDS, I was not really surprised, or panicked. But I did not associate my problem with AIDS because I knew nothing about the disease. My husband, he knew about it. He had heard about it in the newspaper. When I found out that it was a fatal disease and that there was no treatment, I prayed to God and accepted it. I immediately told my mother and my husband. My mother dropped everything to come and see me in the hospital.
"Since then, I've been going regularly to my HIV consultations and I joined an association of people living with AIDS. Two months ago, during a consultation, I was told that I could receive a treatment that would help me regain my health and strength. They also explained that I would not be cured but "stabilized." I was very happy and came to the clinic three times before I took my first medication, because I don't know how to read and they had to give me long explanations.
"At that time, I remember I was weak and had difficulty moving about. I often had diarrhea and headaches; I was sore all over and had a dry mouth. I also had difficulty doing things around the house: cleaning, washing, sweeping the front of the house and cooking. Life was very difficult because our income dropped significantly while I was ill. For three years, I did practically nothing. My husband's income is not constant as he is a seasonal worker. He works on farms in the north of the country picking tobacco. He's away for five to six months of the year and sends us money.
"Since I started the treatment, I've been feeling better and better—it's miraculous! I can fetch wood for the fire and I can even walk to the hospital on my own, which is two hours away on foot. Taking my medication twice a day and going to the hospital once a week is not a constraint because I am fully aware that this treatment is saving my life.
"Another thing is that the people around me didn't know that I have AIDS. But the word got out and, at the beginning, I was rejected. My neighbours and friends came less and less often to visit me. Some even did not come for fear that they might be infected by simple contact. My mother told me not to worry and to let people talk. I was able to make new friends in the association where I'm a member. We see each other often and are very supportive because we all have the same disease. Since I started treatment, people see that I'm getting better, so they have started to visit me again. I think they pay more attention to my appearance than the disease itself. By taking on the appearance of a healthy person, I can find my place in society again. I don't resent people's attitudes. To me, it's more important that I have my life back again."
Fred2
Fred is 42 years old. He is a small man, very courteous and gentle. A week ago, he suffered from headaches and a stiff neck. Suspected of having meningitis, he underwent a lumbar puncture which kept him in hospital. Today, he's better; he's smiling and seems to have more energy, and sits surrounded by his two sons. The eldest is his father's "guardian." Fred explains how he found out he was HIV-positive and the effect of his triple therapy.
"I started getting ill in 1997. I had a fever, I felt weak, I was dizzy and my limbs were itchy and sore. I was admitted to the hospital in December 2000 because I was very ill. I stayed a month and had to stop a working. It was a disaster. I'm a farmer and no one could replace me. My mother is too old, my sons are studying and my neighbors have their own farms to look after. Everything I had planted was lost.
"I had heard of HIV on the radio. They described the symptoms so I made the link to mine. I did my first test in June 2001. Frazer, the counsellor, told me that I had contracted the virus, but that I shouldn't worry, that it didn't mean this was the end of everything. After my test, I went to an HIV clinic. I took medication to get better but it had little effect. Then they told me about ARV treatment. They said it was a treatment that was already being used in England and America. I am very lucky to be able to get ARVs in such a poor country. I immediately agreed to it. Next week, it will be eight weeks since I started treatment. For sure, the treatment is a burden and the hospital is far away. It takes me three hours on foot to get there every week. But it's better than dying. And soon, I'll only need to come once a month to the HIV clinic to take my medication.
"My treatment has made a big change to my life. In fact, at each consultation, they write 'no problem' in my notebook. I don't have a fever anymore and I don't feel sick. I feel good and my body is strong again. I have even put on a bit of weight. But the most important thing is that I've been able to start work again. I'm also going to be able to build a new house. I know that life is going to get better now. People around me are also changing. They say to me, 'You look better. What's going on?' Or they don't talk about it anymore. Yesterday, for example, I was with my brother and some friends came to join us. We started talking, as if nothing had happened. Even if people saw me ill before, they don't see me as being ill today. So they don't talk about it.
"When I found out I had HIV, I immediately told my family. I said to them: 'I have HIV. Watch out, my sons! Watch out! See what happened to me!' I also told my best friend. In my close circle, reactions varied. In fact, there are two categories of persons: those who know how the virus is transmitted and those who are prejudiced. They think that you can catch the disease 'just like that' and they stop coming to see you.
"My counsellor told me about the HIV groups that exist. Taking part in them did me a lot of good. I feel very involved. Actually, I'm going to participate in a training session soon so I can also become a volunteer counsellor and inform young people. It's perfect because I always wanted to be a teacher, but I was never able to continue my studies—I had to work. Now, I want to teach others how to avoid getting infected. People have to understand the danger of this disease and the danger of not protecting yourself. I think that people have to be informed because many only have very vague ideas about it all."
Mary2
Mary is 32 years old. From a very young age, she has suffered from acute polyarthritis, which has paralysed both of her legs. She seems fragile but her face and gaze are determined. Her handshake is incredibly firm.
Mary has come for her weekly ARV treatment at Chiradzulu hospital, as she has done every week for the last month. It takes her four hours to walk there and four hours to walk back.
"Walking is not a big sacrifice for me. It's true that I have to dedicate a whole day each week to going to hospital, but it's vital for me.
"I found out that I was HIV-positive in July last year. I had come to the hospital because my five year old daughter was ill, and the staff suggested I take the HIV test. It was the third time for me—the first time I took it, I was pregnant and it was negative, then I did a second test a few months later. The third, positive result was a real shock to me because I wasn't ill. I didn't expect it at all. I was doubly affected because I also found out that my daughter was HIV-positive. But the MSF counsellor reassured me and told me that treatment existed for the diseases that I might contract.
"I thought about it all and I knew that I was going to die. So I started selling my things one by one, and I stopped going to work on the farm. I was waiting to die.
"My daughter was also infected, so I had no reason to hope. She's my reason for living and as we no longer see her father, what would become of her if I died before her?
"My mother is the only one who knows about my illness. My friends don't know and I don't want them to. I'm part of an association of people living with HIV/AIDS. With their help, I've started to consider talking about it, but I don't feel ready just yet.
"Last month, the MSF doctor told me that I could be treated with ARVs, which would stabilize my illness and allow me to get back some strength. I didn't expect it; it was as much of a surprise as finding out I was HIV-positive.
"I've started to hope again, and I've picked up things that I was doing before I found out that I was HIV-positive. I feel stronger today, I've got some energy back, and I want to continue living and living well. Of course I will continue my treatment. For me it's not an effort but a great and unique opportunity.
"Before, I used to have a little business. I knitted pullovers and sold them. I had stopped everything but I'm going to start again and I'll look for work on a farm so that I can have a fixed income. I also want to expand my home, which I worked to build.
"By going to the HIV Clinic in Thomas, I met this association of AIDS patients I mentioned before. They have helped me a lot and today, I really want it to develop and strengthen so that we can talk about our experience and pass on our message. So that we and other HIV-positives can have a voice."
- UNAIDS, 1999
- Name has been changed for the privacy of the patient



